If you’re considering Mounjaro for weight loss, you may be wondering how it could affect your fertility as a woman. Mounjaro (tirzepatide) is a licensed medication for weight management, but many women are concerned about whether taking Mounjaro might impact their ability to get pregnant.
In this article, we’ll explore what is currently known about Mounjaro and fertility in women. We’ll discuss how this weight loss medication works and what you should consider if you’re planning to conceive while using Mounjaro.
Table of contents
- Key takeaways
- Mounjaro and fertility
- Obesity and fertility
- How obesity affects female fertility: Explained simply
- Obesity: the definition
- Does weight loss improve fertility?
- How obesity affects female hormones and fertility
- How obesity affects sex hormones and insulin
- How weight can affect your periods
- Can Mounjaro help with fertility?
- Does Mounjaro increase fertility?
- The link between Mounjaro and fertility
- Can losing weight improve fertility?
- Is Mounjaro safe when trying to conceive?
- When should you stop taking Mounjaro if you are trying to conceive?
- Summary
- How to get Mounjaro from Courier Pharmacy
- Why buy Mounjaro from Courier Pharmacy?
- References
-
 Mounjaro 15mg Injection£229.99 – £899.99
Mounjaro 15mg Injection£229.99 – £899.99 -
 Mounjaro 5mg Injection£145.99 – £565.99
Mounjaro 5mg Injection£145.99 – £565.99 -
 Mounjaro 2.5mg Injection£145.99 – £565.99
Mounjaro 2.5mg Injection£145.99 – £565.99
Key takeaways
- There is currently limited data on how Mounjaro directly affects fertility or the menstrual cycle. However, weight loss associated with Mounjaro may indirectly improve fertility by addressing issues like hormonal imbalances and insulin resistance, which are linked to excess body weight.
- Maintaining a healthy weight can positively impact menstrual regularity, ovulation, and overall fertility. Excess weight can disrupt hormone levels, reduce egg quality, and increase the risk of pregnancy complications, while extreme weight loss can also negatively affect reproductive health.
- Mounjaro is not recommended during pregnancy due to potential risks to the baby, as suggested by animal studies. It is advised to stop Mounjaro treatment at least two months before trying to conceive and to use additional contraception methods while on the medication, as it may reduce the effectiveness of oral birth control.

Mounjaro and fertility
Mounjaro (tirzepatide) is a medication used for weight management. While there is limited research on its direct effects on fertility, weight loss achieved with Mounjaro can help improve fertility in people with obesity-related reproductive issues.
Excess weight can disrupt hormones, affect ovulation, and make it harder to conceive. By supporting weight loss, Mounjaro may help restore regular menstrual cycles and improve ovulation, both of which are important for fertility.
However, Mounjaro is not specifically approved for fertility treatment, and similar benefits can be seen with other weight loss interventions.

If you are planning to become pregnant or have concerns about fertility while taking Mounjaro, it is important to discuss your plans with your healthcare provider to ensure that the safest and most effective approach for fertility is followed.
Obesity and fertility
It’s well accepted that excess weight and obesity can play a significant role in reproductive health [1]. For many people, this is a key motivation when starting a weight loss journey.
Whether you’re planning for a family, considering getting pregnant soon, or simply wondering how weight loss drugs could affect your birth control, you’re in the right place.
It’s important to mention that research in this area is still emerging, but we’re here to break down what’s currently known and help you make informed decisions.

How obesity affects female fertility: Explained simply
Carrying extra weight doesn’t just impact your general health—it can also make it harder to get pregnant. Many women who are overweight or obese struggle with fertility, and research has shown a clear link between obesity and problems with getting pregnant.
Obesity and ovulation
Obesity can lead to issues like irregular periods, trouble ovulating (releasing an egg), and lower chances of success with fertility treatments. It also raises the risk of miscarriage and can cause complications for both mum and baby during pregnancy [2].
Obesity and fertility: the stats
Studies show that more than 40% of women with irregular periods, infertility, or repeated miscarriages are overweight or obese [1], [2]. Women with obesity are more likely to have hormone imbalances, irregular or missed periods, and problems with ovulation, all of which can make it harder to conceive.

Obesity: the definition
According to the CDC and WHO, a BMI over 25 means you’re overweight, over 30 is considered obese, and over 40 is classed as severely obese [3].
Is the BMI as a measure of obesity outdated?
BMI (Body Mass Index) isn’t a perfect way to measure if someone is healthy or not. Sometimes, it can make people appear healthier or less healthy than they really are, as it only considers weight and height, rather than actual body fat or the overall health of someone’s body.
A large group of experts came together to develop better ways to define and diagnose obesity. They now say:
- Obesity means having too much body fat, which can hurt your organs and lead to serious health problems.
- Clinical obesity is when extra body fat actually causes health issues, like heart disease, diabetes, or makes it hard to do everyday things.
- Preclinical obesity is when someone has extra body fat but isn’t sick yet, though they have a higher risk of getting health problems in the future.
They recommend using more than just BMI to assess obesity, such as measuring your waist circumference. For individuals with a very high BMI (over 40), it’s clear that they have excessive body fat [4].
Doctors should check if someone’s extra body fat is causing real health problems, rather than just looking at the numbers. People with health problems from obesity should get proper treatment. People who aren’t sick yet but have excess body fat should receive advice and support to help prevent future health problems.
Fat shaming
The experts also say we shouldn’t blame people for having obesity, and that health workers need training to avoid treating people unfairly. Their new advice is supported by numerous health organisations worldwide.

Does weight loss improve fertility?
Doctors generally recommend that women who are overweight or obese try to lose weight—especially around the belly—before starting fertility treatments. Even a small amount of weight loss can help improve your chances of getting pregnant.
Studies in humans have shown that losing weight with medical help can improve fertility. The most important factor is how much weight you lose overall. Research suggests that losing just 5% of your starting body weight (approximately 5–6 kg for many individuals) can significantly improve your chances of getting pregnant [5].
It’s best to lose this weight over a period of about 4 to 6 months (16 to 26 weeks), as taking a bit more time seems to lead to better results [5]. The benefits of this weight loss include better hormone balance, more regular menstrual cycles, improved ovulation, and increased chances of getting pregnant.

How obesity affects female hormones and fertility
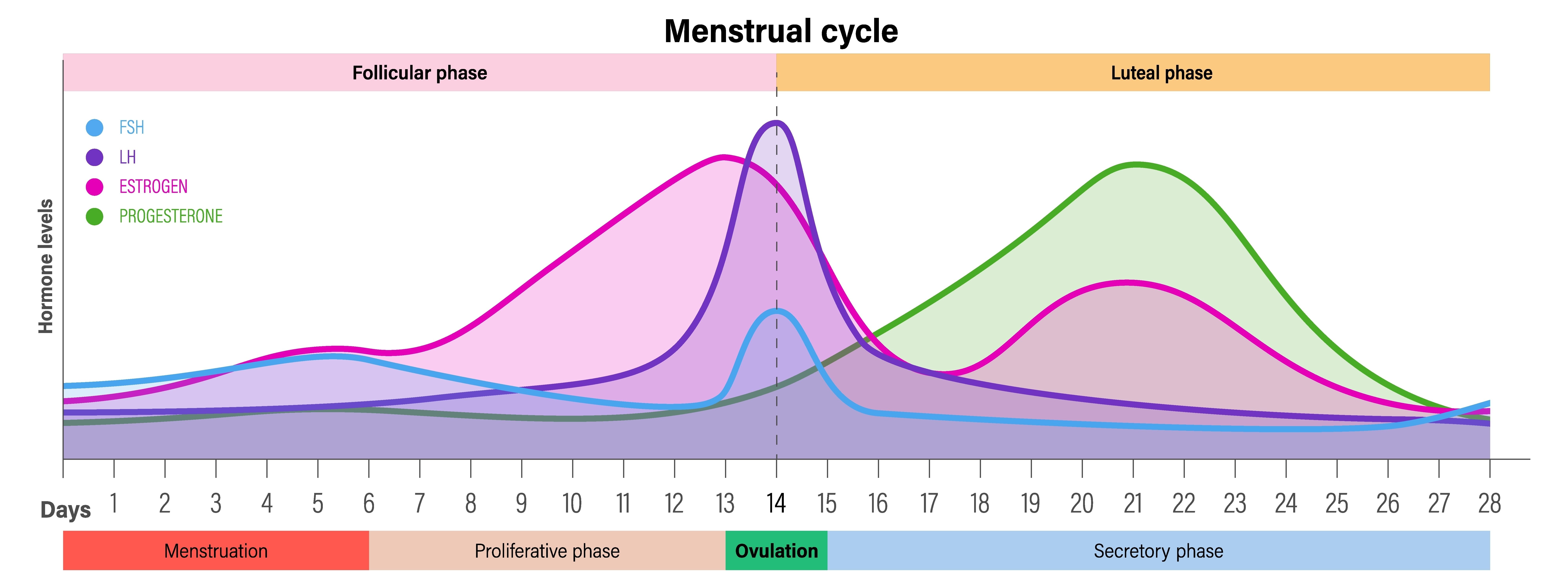
Obesity can upset the balance of important hormones that control a woman’s reproductive system, known as the hypothalamic–pituitary–ovarian (HPO) axis. Too much body fat can cause this system to work less effectively in several ways.
- Early puberty: Girls who are overweight or obese often go through puberty earlier than those at a healthy weight, while very thin girls might experience delayed puberty [6].
- Hormone changes: Women with obesity often have higher levels of certain hormones, like luteinizing hormone (LH), androstenedione, and estrone, as well as higher insulin and certain blood fats. They also tend to have lower levels of “good” cholesterol [7].
- Leptin’s role: Leptin is a hormone made by fat tissue [8]. The more body fat you have, the more leptin you produce. Leptin helps signal the start of puberty and affects fertility. However, too much leptin (as seen in obesity) can disrupt the normal function of the ovaries and make it harder to get pregnant, even reducing the chances of success with treatments like IVF [9].
- Ovulation problems: High leptin levels can interfere with the ovaries’ ability to produce hormones and release eggs, which directly impacts fertility [10].
- Insulin resistance: Obesity can also cause the body to become resistant to insulin, another hormone. This can further disturb the balance of reproductive hormones and make it harder to conceive [11].
In short, carrying extra body fat can throw off the delicate hormone balance needed for normal periods and ovulation, making it more difficult for women to get pregnant.

How obesity affects sex hormones and insulin
When someone is obese, their body makes more sex hormones like oestrogen and testosterone. This happens because fat tissue not only produces these hormones but also changes some hormones from one type to another. As a result, there’s more oestrogen and androgen (male-type hormones) in the body [12].

Obesity and SHBG
Obesity also lowers the amount of a protein called SHBG, which normally helps control how much of these hormones are active. With less SHBG, more hormones are free to affect the body’s tissues [13].
These hormone changes can begin as early as the teenage years and are particularly common in individuals who carry excess weight around their midsection. This imbalance can cause problems with the ovaries, making it harder for women to ovulate (release eggs) and get pregnant.

Insulin resistance and obesity
Obesity also causes the body to become resistant to insulin, a hormone that regulates blood sugar levels. As a result, the body makes even more insulin, which can trigger the ovaries to produce more male hormones. This creates a cycle that further disrupts the balance of sex hormones, leading to irregular periods, problems with ovulation, and reduced fertility [10].
Hormones and obesity summary
Being overweight, especially around the belly, can upset hormone and insulin levels, making it harder for women to have regular periods and get pregnant.

How weight can affect your periods
What we do know for sure is that weight loss and maintaining a healthy weight can have a big impact on your periods and fertility.
Being overweight or living with obesity can cause menstrual changes, such as:
- irregular periods [14],
- heavier bleeding, and
- a higher chance of experiencing PMS or PMDD.
Insulin resistance and your periods
Carrying extra weight is also associated with high blood sugar, insulin resistance, and hormonal imbalances.
Insulin resistance happens when your body doesn’t respond properly to insulin, the hormone that helps control blood sugar. In response, your pancreas works overtime to produce even more insulin.
This can disrupt hormone balance and blood sugar levels, which often disrupts your menstrual cycle too.”
A recent Chinese study found an association with insulin resistance and menstrual irregularities in women with PCOS [15].

Fat, oestrogen and your periods
It’s not just your ovaries that can produce oestrogen. Your fat cells can also produce oestrogen, and in women with more body fat, these cells release extra oestrogen.
This is due to an enzyme in fat tissue called aromatase, which turns other hormones, such as testosterone, into oestrogen [16].
When there’s a lot of oestrogen in the body, it can confuse the brain and stop it from sending the right signals to the ovaries.
These signals — hormones called LH and FSH — are needed for regular periods and ovulation. High oestrogen levels can make the body think it’s already pregnant, even when it’s not. This can lead to missed periods or irregular cycles [17].

Weight loss improves your menstrual cycles
Losing weight in a healthy way can help make your cycle more regular, improve insulin resistance, and balance your hormones.
Weight loss improves ovulation
Five large studies found that women with overweight or obesity who lost about 7% of their body weight (around 9 to 20 pounds) were more likely to start ovulating again and conceive naturally. These results came from trials with over 100 women in each study who were trying to induce ovulation [18].

Rapid weight loss and your periods
OK, so losing weight can help improve your periods, but what happens if you lose too much weight?
Losing weight too quickly or being underweight can also disrupt your hormones, sometimes causing periods to stop.
When your body doesn’t have enough nutrients or fat, oestrogen levels can drop, and ovulation may stop, leading to irregular or absent periods.

Functional Hypothalamic Amenorrhea (FHA)
FHA is when a woman stops having periods because of low body fat, too much exercise, or high stress. The brain slows down the hormones needed for ovulation, often as a way to conserve energy. This is common in athletes or women who lose weight quickly.
The body sees low fat as a sign that it’s not a safe time to get pregnant, so it shuts down the cycle. Hormones like leptin (from fat) and cortisol (from stress) are involved [19].
FHA is diagnosed after ruling out other causes, like thyroid issues or PCOS.

How much stored fat is needed for periods?
To start their first period (menarche), a girl needs to have at least 17% body fat. For regular monthly periods to continue, around 22% body fat is required [19].
Treatment usually focuses on eating more, exercising less, and reducing stress to restore the natural hormone balance.

Can Mounjaro help with fertility?
Before we dive into looking at the evidence, we will have a quick recap on what Mounjaro is and how it works.
What is Mounjaro, and how does it work?
Mounjaro is a medicine made by a company called Eli Lilly. Its main ingredient is tirzepatide. This medicine works by copying two natural hormones in your gut, called GLP-1 and GIP [20].
These hormones help your body by:
- Making you feel less hungry
- Helping you feel full after eating
- Slowing down how quickly your stomach empties
Because Mounjaro uses both GLP-1 and GIP, people sometimes call it a “twincretin.” Early studies in mice showed that this mix helped them lose more weight [21]. Later, big studies in people proved that Mounjaro can help with weight loss, too.
The table below shows what GLP-1 and GIP do in the body.
How effective is Mounjaro for weight loss?
The SURMOUNT-4 trial was a big study that lasted for 72 weeks. It looked at how well Mounjaro works for people who are very overweight. The results showed that people taking the highest dose of Mounjaro 15mg lost, on average, about 24% of their body weight. More than 8 out of 10 people in the study lost over 15% of their weight [22].
These results are much better than what we’ve seen with other weight loss medicines. For example, the drug semaglutide usually helps people lose between 10 and 15 kilograms. But Mounjaro can help people lose up to 24 kilograms, making Mounjaro the most effective medicine for weight loss… so far.
Does Mounjaro increase fertility?
To date, no studies have looked at Mounjaro’s ability to increase fertility; however, studies with other GLP-1 receptor agonists, like semaglutide, and their effects on women with polycystic ovary syndrome (PCOS), a common cause of infertility, have been studied.

Direct Studies on Fertility and PCOS
Several studies have looked at how GLP1-RAs help women with PCOS, a common cause of infertility.
One trial discovered that women with obesity and PCOS who took liraglutide had more regular periods and higher conception rates than those who did not [23].
Another study found that women who took liraglutide with metformin had a much higher pregnancy rate during IVF than those who took metformin alone (85.7% vs 28.6%) [24].
Researchers believe the benefits come from both weight loss and possible direct effects on the ovaries and womb, as GLP-1 receptors are found in the reproductive system [25]. GLP1-RAs may reduce inflammation and improve the health of the ovaries and uterus, which is important for women with PCOS or obesity.
Another big review looked at 11 studies with 840 women and found that medicines called GLP-1 receptor agonists (GLP1-RAs) helped improve natural pregnancy rates and made periods more regular [26].
While the total pregnancy rates and IVF pregnancy rates were similar between women who took GLP1-RAs and those who did not, the chance of getting pregnant soon after starting GLP1-RAs was higher in some groups [26].
Women taking GLP1-RAs also had better insulin sensitivity, lower BMI, smaller waist size, higher levels of sex hormone binding globulin, and slightly lower total testosterone—all changes that can help improve fertility [26].

The link between Mounjaro and fertility
There isn’t a lot of robust evidence yet about whether Mounjaro affects fertility despite women sharing stories about becoming pregnant while on Mounjaro on social media [27].
Scientists are still studying this, so we don’t know for sure if Mounjaro has any direct effect on fertility.
What we do know is that weight and fertility are closely linked, and losing weight can sometimes help improve fertility for some people.
If you’re thinking about getting pregnant or have questions about fertility while taking Mounjaro, it’s important to talk to your doctor for advice that’s right for you.

Can losing weight improve fertility?
Carrying extra weight can make it harder to get pregnant. This is because it can upset your periods and mess with your hormones. But being overweight can affect fertility in several ways, such as:
- Raising certain male hormones in the body, which can stop ovulation (the release of eggs)
- Causing problems with how your body makes hormones
- Affecting how your body uses energy, which can impact the ovaries
- Lowering the quality of eggs and making it less likely for an egg to be fertilised [28]
There isn’t one “perfect” weight for getting pregnant, because everyone is different. But being overweight—or even underweight—can make it harder to conceive naturally.
Extra body weight can also make fertility treatments more difficult. It can lower the chances of success and make it harder to collect eggs. There may also be fewer healthy embryos and a higher risk of problems during treatment [28].
The good news is that losing weight healthily and steadily can help improve fertility. Weight loss injections like Mounjaro, when used as part of a bigger plan, can help you reach a healthier weight. This can make it easier to become pregnant.
Even losing just 5% of your body weight can make a difference. Getting to a healthier weight can help your body ovulate and boost your chances of getting pregnant, whether naturally or with fertility treatment [5].
Is Mounjaro safe when trying to conceive?
Now that we’ve talked about how weight loss could potentially improve fertility, what should you do if you’re taking Mounjaro and want to have a baby?
Pregnancy and safety studies
So far, there is little evidence that GLP1-RAs such as Mounjaro cause harm to the baby if taken early in pregnancy. Still, most guidelines recommend stopping these medicines before trying to conceive.
Animal studies have shown some risks, but recent human studies [29] found no increase in birth defects in women who accidentally took GLP1-RAs during the first trimester.
Most of what we know about medicines like Mounjaro in pregnancy comes from women who became pregnant by accident while taking part in medical studies [30].
Right now, there isn’t enough research to know how Mounjaro affects pregnant people or unborn babies. We also don’t know if the medicine can pass into breast milk [31].
So, based on the lack of robust evidence regarding the safety of Mounjaro in pregnancy, experts say it’s safest to stop these medicines at least 2 months before getting pregnant, and not to use them while breastfeeding.

When should you stop taking Mounjaro if you are trying to conceive?
You should stop taking Mounjaro at least 2 months before trying to get pregnant. This gives your body time to clear out the medicine and lowers any possible risks.
Also, it’s important to remember that Mounjaro can make birth control pills less effective [32]. So, it’s recommended to use condoms or another non-pill birth control for at least a month after starting Mounjaro and after each time you increase your dose [32].

Summary
- Mounjaro is a medicine used to help people lose weight.
- There isn’t strong proof yet that Mounjaro directly improves fertility.
- Losing extra weight can sometimes make it easier to get pregnant.
- If you want to use Mounjaro and are thinking about having a baby, talk to your doctor for advice that suits you.
-
 Mounjaro 12.5mg Injection£229.99 – £899.99
Mounjaro 12.5mg Injection£229.99 – £899.99 -
 Mounjaro 10mg Injection£185.99 – £735.99
Mounjaro 10mg Injection£185.99 – £735.99 -
 Mounjaro 7.5mg Injection£185.99 – £735.99
Mounjaro 7.5mg Injection£185.99 – £735.99
How to get Mounjaro from Courier Pharmacy
- Fill out the online form
Start by answering some questions online. This helps our team check if Mounjaro is right and safe for you. - Upload a photo
You’ll need to send us a clear, recent photo of yourself. This is for your safety and to confirm who you are. - Show proof for higher doses
If you want a higher dose, you’ll need to show proof—like photos of your old pens or a record from your doctor—that you have safely worked up to that dose. - Provide your GP’s details
Share your GP’s contact information so we can keep your doctor updated about your treatment. - Arrange a video call
You’ll need to join a video call with our clinical team. This is to make sure you’re using Mounjaro safely and to answer any questions you might have.

Why buy Mounjaro from Courier Pharmacy?
- Great prices—get Mounjaro at some of the best prices online.
- Free sharps bin for safe disposal of used pens.
- Free needles and alcohol wipes are included with every order.
- All consultations are free, from your first assessment to ongoing support.
- We can provide extra medicine if you have side effects that are hard to manage.
- Our team is friendly and here to help you every step of the way.
If you have any questions or need help, contact us—we’re here for you!
Our Courier Pharmacy team created this content to provide general information and is not a substitute for professional medical advice. For personalised recommendations about your health, always consult with your doctor or contact us to speak with one of our prescribers.

References
- Amiri, M. and Tehrani, F.R., 2020. Potential adverse effects of female and male obesity on fertility: a narrative review. International journal of endocrinology and metabolism, 18(3), p.e101776.
- Slopien, R., Horst, N., Jaremek, J.D., Chinniah, D. and Spaczynski, R., 2019. The impact of surgical treatment of obesity on female fertility. Gynaecological Endocrinology, 35(2), pp.100-102.
- Chooi, Y.C., Ding, C. and Magkos, F., 2019. The epidemiology of obesity. Metabolism, 92, pp.6-10.
- Rubino, F., Cummings, D.E., Eckel, R.H., Cohen, R.V., Wilding, J.P., Brown, W.A., Stanford, F.C., Batterham, R.L., Farooqi, I.S., Farpour-Lambert, N.J. and le Roux, C.W., 2025. Definition and diagnostic criteria of clinical obesity. The Lancet Diabetes & Endocrinology.
- Pavli, P., Triantafyllidou, O., Kapantais, E., Vlahos, N.F. and Valsamakis, G., 2024. Infertility improvement after medical weight loss in women and men: a review of the literature. International journal of molecular sciences, 25(3), p.1909.
- Castellano, J.M., Bentsen, A.H., Sanchez-Garrido, M.A., Ruiz-Pino, F., Romero, M., Garcia-Galiano, D., Aguilar, E., Pinilla, L., Dieguez, C., Mikkelsen, J.D. and Tena-Sempere, M., 2011. Early metabolic programming of puberty onset: impact of changes in postnatal feeding and rearing conditions on the timing of puberty and development of the hypothalamic kisspeptin system. Endocrinology, 152(9), pp.3396-3408.
- Al-Yasiry, R.Z., Jwad, M.A., Hasan, M.F. and Al-Sayigh, H.A., 2022. How obesity affects female fertility. Medical Journal of Babylon, 19(2), pp.111-114.
- Friedman, J.M., 1998. Leptin, leptin receptors, and the control of body weight. Nutrition reviews, 56(suppl_1), pp.S38-S46.
- Broughton, D.E. and Moley, K.H., 2017. Obesity and female infertility: potential mediators of obesity’s impact. Fertility and sterility, 107(4), pp.840-847.
- Gambineri, A., Laudisio, D., Marocco, C., Radellini, S., Colao, A., Savastano, S. and Obesity Programs of nutrition, Education, Research and Assessment (OPERA) group, 2019. Female infertility: which role for obesity?. International journal of obesity supplements, 9(1), pp.65-72.
- Van Leckwyck, M., Kong, W., Burton, K.J., Amati, F., Vionnet, N. and Pralong, F.P., 2016. Decreasing insulin sensitivity in women induces alterations in LH pulsatility. The Journal of Clinical Endocrinology & Metabolism, 101(8), pp.3240-3249.
- Santoro, N., Torrens, J., Crawford, S., Allsworth, J.E., Finkelstein, J.S., Gold, E.B., Korenman, S., Lasley, W.L., Luborsky, J.L., McConnell, D. and Sowers, M.F., 2005. Correlates of circulating androgens in mid-life women: the study of women’s health across the nation. The Journal of Clinical Endocrinology & Metabolism, 90(8), pp.4836-4845.
- Pasquali, R. and Gambineri, A., 2006. Metabolic effects of obesity on reproduction. Reproductive biomedicine online, 12(5), pp.542-551.
- Ju, H., Jones, M. and Mishra, G.D., 2015. A U-shaped relationship between body mass index and dysmenorrhea: a longitudinal study. PloS one, 10(7), p.e0134187.
- Niu, J., Lu, M. and Liu, B., 2023. Association between insulin resistance and abnormal menstrual cycle in Chinese patients with polycystic ovary syndrome. Journal of Ovarian Research, 16(1), p.45.
- Dos Santos, B.R., Casanova, G., da Silva, T.R., Oppermann, K. and Spritzer, P.M., 2024. Association between the aromatase (CYP19A1) gene variant rs10046 and cardiovascular risk in postmenopausal women. Archives of Endocrinology and Metabolism, 68(spe 1), p.e240087.
- De Pergola, G., Tartagni, M., d’Angelo, F., Centoducati, C., Guida, P., Giorgino, R. (2009). Abdominal fat accumulation, and not insulin resistance, is associated with oligomenorrhea in non-hyperandrogenic overweight/obese women. Journal of Endocrinological Investigation; 32(2): 98–101.
- Goldberg, A.S. and Boots, C.E., 2024. Treating obesity and fertility in the era of glucagon-like peptide 1 receptor agonists. Fertility and Sterility.
- Huhmann, K., 2020. Menses requires energy: a review of how disordered eating, excessive exercise, and high stress lead to menstrual irregularities. Clinical therapeutics, 42(3), pp.401-407.
- Medical Mojo (n.d.) Mounjaro Side Effects: What You Need to Know. Available at: https://medicalmojo.co.uk/mounjaro-side-effects/#h-what-is-mounjaro (Accessed: 22 June 2025).
- Coskun, T., et al. (2018). Tirzepatide, a dual GLP-1 and GIP receptor agonist, induces significant weight loss in patients with obesity. Diabetes Care, 41(10), 2100–2108.
- ClinicalTrials.gov (2020) A Study of Tirzepatide (LY3298176) in Participants With Obesity or Overweight (SURMOUNT-1). Available at: https://clinicaltrials.gov/study/NCT04660643 (Accessed: 22 June 2025).
- Elkind-Hirsch, K., Marrioneaux, O., Bhushan, M., Vernor, D. and Bhushan, R., 2008. Comparison of single and combined treatment with exenatide and metformin on menstrual cyclicity in overweight women with polycystic ovary syndrome. The Journal of Clinical Endocrinology & Metabolism, 93(7), pp.2670-2678.
- Jensterle, M., Herman, R. and Janež, A., 2022. Therapeutic potential of glucagon-like peptide-1 agonists in polycystic ovary syndrome: from current clinical evidence to future perspectives. Biomedicines, 10(8), p.1989.
- Bednarz, K., Kowalczyk, K., Cwynar, M., Czapla, D., Czarkowski, W., Kmita, D., Nowak, A. and Madej, P., 2022. The role of Glp-1 receptor agonists in insulin resistance with concomitant obesity treatment in polycystic ovary syndrome. International journal of molecular sciences, 23(8), p.4334.
- Zhou L, Qu H, Yang L, Shou L. Effects of GLP1RAs on pregnancy rate and menstrual cyclicity in women with polycystic ovary syndrome: a meta-analysis and systematic review. BMC Endocr Disord. 2023 Nov 8;23(1):245.
- Merhi, Z., Karekar, M. and Mouanness, M., 2025. GLP-1 receptor agonist for weight loss and fertility: Social media and online perception versus evidence-based medicine. PloS one, 20(7), p.e0326210.
- Da?, Z.Ö. and Dilbaz, B., 2015. Impact of obesity on infertility in women. Journal of the Turkish German Gynecological Association, 16(2), p.111.
- Dao K, Shechtman S, Weber-Schoendorfer C, Diav-Citrin O, Murad RH, Berlin M, Hazan A, Richardson JL, Eleftheriou G, Rousson V, Diezi L, Haefliger D, Simões-Wüst AP, Addor MC, Baud D, Lamine F, Panchaud A, Buclin T, Girardin FR, Winterfeld U. Use of GLP1 receptor agonists in early pregnancy and reproductive safety: a multicentre, observational, prospective cohort study based on the databases of six Teratology Information Services. BMJ Open. 2024 Apr 24;14(4):e083550.
- Parker, C.H., Slattery, C., Brennan, D.J. and le Roux, C.W., 2025. Glucagon?like peptide 1 (GLP?1) receptor agonists’ use during pregnancy: Safety data from regulatory clinical trials. Diabetes, Obesity and Metabolism.
- Organization of Teratology Information Specialists (OTIS) (2024) Tirzepatide (Mounjaro®, Zepbound®) – MotherToBaby Fact Sheet. In: MotherToBaby | Fact Sheets [Internet]. Brentwood (TN): OTIS. Available at: https://www.ncbi.nlm.nih.gov/books/NBK605070/ (Accessed: 12 July 2025).
- Courier Pharmacy (2024) Mounjaro and contraception: what you need to know. Available at: https://courierpharmacy.co.uk/mounjaro-and-contraception/ (Accessed: 22 June 2025).