Mast cell activation syndrome (MCAS) is a condition that’s still flying under the radar for many people, yet it can have a big impact on everyday life. This guide will break down what MCAS means, why it happens, how doctors figure it out, and what you can do if you think you’re affected. We’ll keep things simple, trustworthy, and a bit light-hearted—because understanding your health should never be intimidating.
Table of contents
- Five key takeaways:
- Who is this article for, and why should you care?
- What is mast cell activation syndrome?
- What are the symptoms of MCAS?
- What are mast cells?
- What do mast cells do, and why do they sometimes go haywire?
- Who can get MCAS?
- What causes mast cell activation syndrome or MCAS?
- What chemicals do mast cells release?
- What are mast cells triggers?
- What can trigger MCAS symptoms?
- Food and specialist diets for mast cell activation syndrome or MCAS
- Low-histamine diets: What do we really know?
- How is MCAS diagnosed?
- How is mast cell activation syndrome treated?
- What else should I know about MCAS?
- Why does mast cell activation syndrome matter?
- MCAS in summary
- What’s the risk of anaphylaxis with MCAS?
- FAQs: What is mast cell activation syndrome? (and other common questions)
- The bottom line: What is mast cell activation syndrome?
- References
-
 Zaditen Elixir – Ketotifen 1mg/5ml Elixir, 300mlPrice range: £34.99 through £99.99
Zaditen Elixir – Ketotifen 1mg/5ml Elixir, 300mlPrice range: £34.99 through £99.99 -
 Ketotifen 1mg (Zaditen) tabletsPrice range: £29.99 through £89.99
Ketotifen 1mg (Zaditen) tabletsPrice range: £29.99 through £89.99 -
 Loratadine 10mg TabletsPrice range: £1.99 through £12.99
Loratadine 10mg TabletsPrice range: £1.99 through £12.99
Five key takeaways:
- MCAS happens when mast cells in your body release chemicals too frequently or in response to harmless things, causing all sorts of symptoms [1].
- Symptoms can show up in many different ways—skin, gut, breathing, and more—making MCAS challenging to diagnose [2].
- Triggers are highly personal; common ones include food, scents, stress, and even weather changes [1].
- Diagnosis usually involves tracking symptoms, trying medications, running lab tests, and ruling out other causes [3].
- Managing MCAS means learning your triggers, working with healthcare pros, and sometimes using medication [2].

Who is this article for, and why should you care?
This article is for anyone who’s puzzled by unexplained allergic reactions, ongoing tiredness, or a strange mix of symptoms that don’t seem to fit together.
It’s also for family members, healthcare professionals, or anyone interested in why MCAS is getting more attention lately. If you want clear, practical information (without the medical jargon), you’re in the right place!

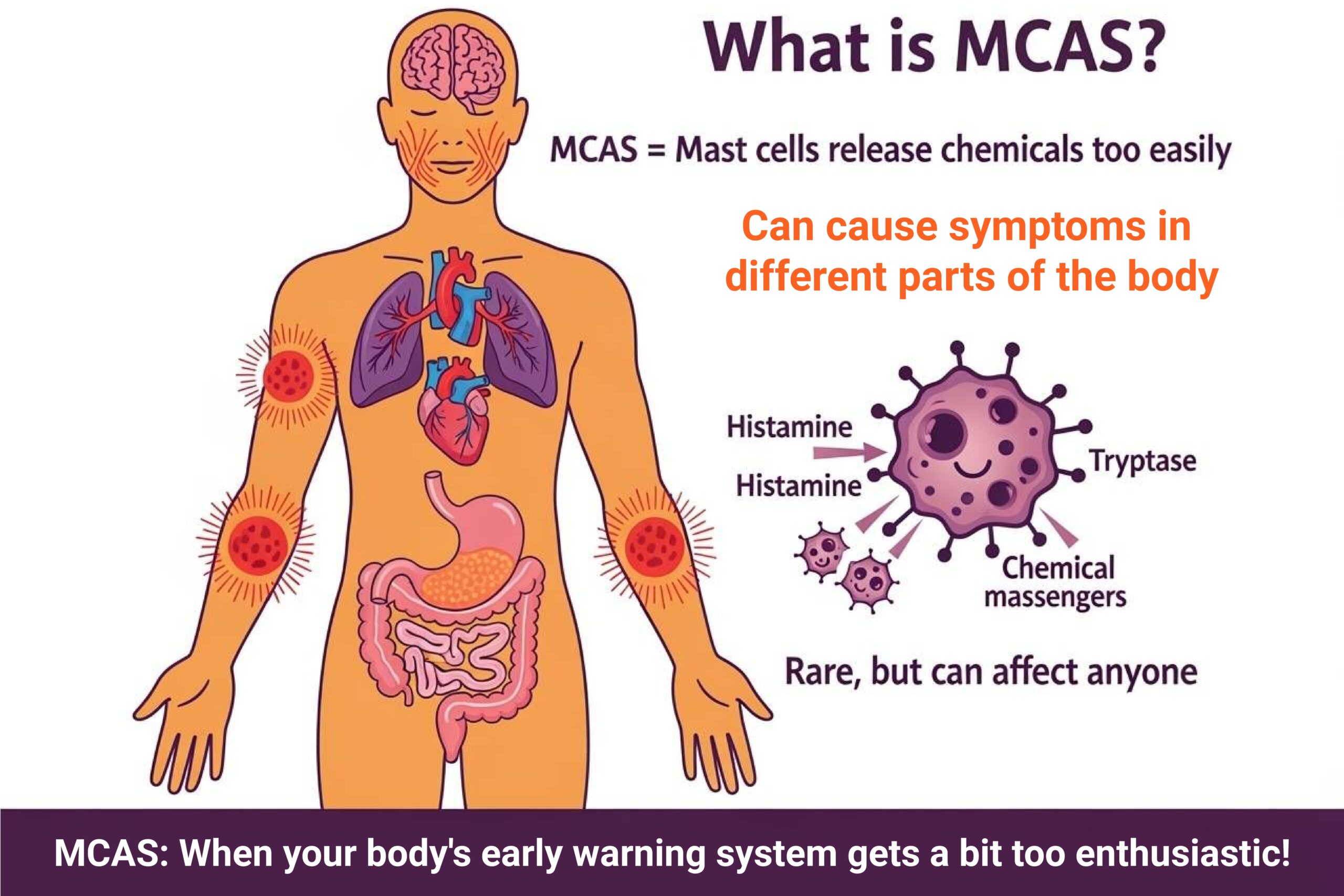
What is mast cell activation syndrome?
Mast cell activation syndrome (MCAS) describes a situation where certain immune cells—mast cells—go into overdrive, releasing their chemical messengers (like histamine and tryptase) too often or in response to things that wouldn’t usually be a problem [1].
Fortunately, it is a rare condition that can cause a range of symptoms in the body. It happens when certain white blood cells, called mast cells, become overactive and release too many chemicals. These chemicals are usually meant to help protect you, but when they’re released too often, they can cause problems.
What are the symptoms of MCAS?
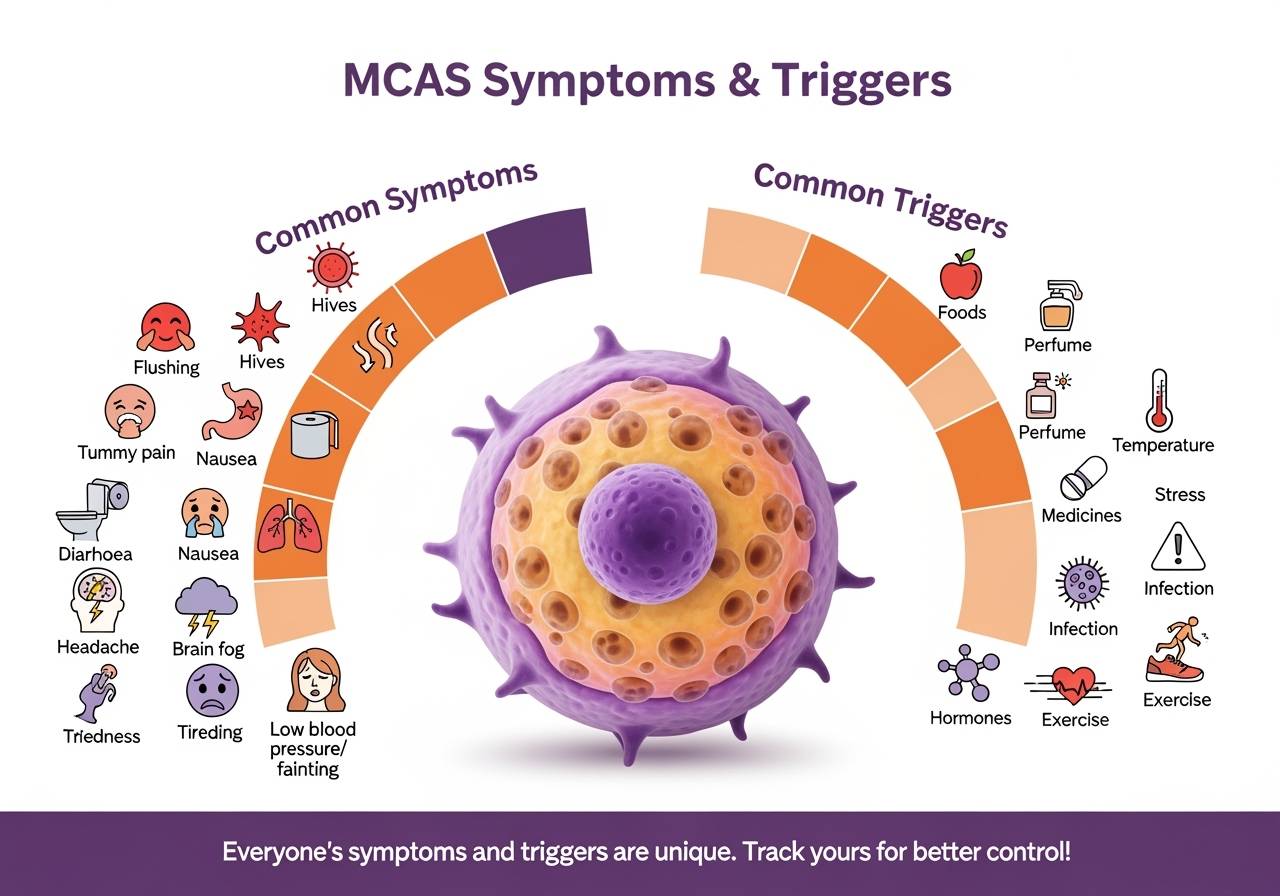
Symptoms can be very different from person to person, and they can come and go. Common symptoms include [1], [2]:
- Flushing (redness of the skin)
- Low blood pressure or fainting
- Hives or swelling
- Headaches
- Nausea, vomiting, or diarrhoea
- Tummy pain
- Wheezing or shortness of breath
- Brain fog or tiredness
Symptoms can affect the skin, stomach, heart, lungs, and even the brain. Sometimes, people have mild symptoms for years, then suddenly get worse after an illness or operation.
MCAS is part of a group of mast cell disorders, which also includes conditions like mastocytosis and hereditary alpha tryptasemia syndrome (HATS) [1]. Some people might even have more than one of these at once.

What are mast cells?
Mast cells are a special type of white blood cell that help protect your body as part of your immune system [4]. They help your body heal, fight infections, and repair tissues [4]. Mast cells store and release different chemicals, especially during allergic reactions [4].
Because they play a big part in emergencies like severe allergic reactions (anaphylaxis), scientists have studied them closely.
Sometimes, mast cells don’t work as they should. In mast cell activation syndrome (MCAS), there can be too many mast cells, or they don’t die off when they should, which means they can cause problems in different parts of the body.
Basically, in MCAS, mast cells get “trigger-happy” and release chemicals even when they don’t need to. This can lead to allergy-like symptoms and affect many parts of the body [2].

What do mast cells do, and why do they sometimes go haywire?
Think of mast cells as your body’s early warning system, always on patrol in places like your skin, lungs, and gut [4]. When they spot something suspicious—like bacteria or an injury—they release chemicals to help you heal.
But with MCAS, these cells can get a bit too enthusiastic, reacting to harmless triggers such as certain foods, perfumes, or even a temperature drop [1], [2].

Who can get MCAS?
MCAS is rare and can happen to anyone at any age. It affects both men and women equally. Scientists don’t yet know exactly how common it is, because it’s often hard to diagnose and may be mistaken for other illnesses.

What causes mast cell activation syndrome or MCAS?
The exact cause isn’t fully understood. Sometimes, MCAS is linked to changes in certain genes, but not always. In MCAS, mast cells don’t multiply too much (like in some other diseases), but they do become too active [5].

What chemicals do mast cells release?
Mast cells are like tiny chemical factories. They produce:
- Histamine: Causes itching, swelling, and redness (classic allergy signs)
- Cytokines: Help with healing and fighting off infection
- Tryptase: An enzyme that’s a marker for mast cell activity
Usually, these chemicals keep you healthy. But with MCAS, they’re released too easily, leading to a range of symptoms [1], [2].

What are mast cells triggers?
If you have MCAS, daily life can sometimes feel tricky because so many things might set off your symptoms.
Mast cells in MCAS are extra sensitive and can react to all sorts of triggers—even things that don’t bother most people [2]. When this happens, your body releases chemicals like histamine, which can cause symptoms in different parts of your body.
Everyone’s triggers are different. Some people know exactly what sets them off, while others find their reactions are unpredictable and can change from day to day.
That’s why it’s really helpful to learn about your own triggers. Figuring out what affects you can help you avoid flares and feel more confident in your daily routine.

What can trigger MCAS symptoms?
People with MCAS can react to many different things. Triggers are anything that makes mast cells release their chemicals. Sometimes, just one thing is enough to cause a reaction. Other times, it’s a mix of small triggers that together push your body over its limit.
What causes symptoms one day might not cause any trouble another day—things like stress, illness, or being exposed to several triggers at once can all make a difference.
Common triggers include:
- Certain foods
- Smells or fragrances
- Changes in temperature
- Medicines or supplements
- Emotional or physical stress
- Infections
- Hormone changes
- Exercise or even pressure on the skin
Some people only react to a few things, while others find that many parts of daily life can set off their symptoms. It takes time to work out your unique set of triggers, but doing so can really help you feel better.
Food and specialist diets for mast cell activation syndrome or MCAS
For many people with MCAS, foods are a common trigger. Sometimes it’s easy to spot which food is causing problems, but often it’s not clear, especially since we usually eat lots of foods together. Reactions can also be delayed by a few days, making it harder to figure out.
Some diets that people with MCAS find helpful include:
- Low histamine
- Dairy free
- Gluten free
- Low salicylates
- Low oxalates
- Low FODMAP
- Low sugar (ketogenic)
- Or a mix of these
If you want to try an elimination diet, it’s important to do so with help from a healthcare professional. Usually, you remove a food group for about six weeks, then slowly add foods back one at a time to see if they cause symptoms. For children, always work with a healthcare provider before making any changes to their diet.

Low-histamine diets: What do we really know?
A low-histamine diet is often recommended for people who struggle with histamine intolerance, such as MCAS.
The idea is simple: avoid foods that are high in histamine. But in reality, there’s no clear agreement about which foods should be left out. Different low-histamine diets can have very different lists of foods to avoid.

What foods are usually excluded?
One thing all experts agree on: fermented foods (like aged cheese, cured meats, sauerkraut, wine, and beer) are high in histamine and should be avoided. These foods can build up lots of histamine because of the way they’re made [6].
Some diets also recommend avoiding certain fish, especially if they’re not super fresh, because histamine can rise quickly when fish isn’t stored well.
Other foods like tomatoes, spinach, and eggplant can have some histamine, especially if they’ve been stored for a while.

Why are some foods on the “avoid” list if they don’t have much histamine?
Surprisingly, many foods that get excluded from low-histamine diets don’t actually contain much histamine.
Some, like citrus fruits and bananas, have other natural chemicals (like putrescine) that might make it harder for your body to break down histamine [6].
For other foods—like chocolate, strawberries, and nuts—there’s a theory that they might cause your body to release its own histamine, but there isn’t strong proof for this yet [7].

Is there a perfect low-histamine food list?
Not really. Only about one-third of foods commonly excluded actually have high histamine levels. This means that a lot of the “rules” for low-histamine diets are based on tradition or guesswork, not hard science. Some people find they react to foods with very little histamine, and researchers think this might be due to other ingredients or how foods interact with our bodies.

What’s the takeaway?
- Avoid fermented foods—they’re the primary source of histamine.
- Be careful with fish unless it’s very fresh.
- Some fruits, veggies, and other foods might cause problems for some people, but not everyone.
- There’s no one-size-fits-all list, and what works for one person might not work for another.
- More research is needed to really understand which foods are safe and which are not.
If you’re thinking about a low-histamine diet, it’s always best to work with a healthcare professional to find out what works for you.

Low histamine foods
- Fresh, unprocessed meats (chicken, turkey, lamb, beef—cooked soon after purchase)
- Freshly caught fish (not canned, smoked, or processed)
- Eggs
- Most fresh fruits (except strawberries, bananas, avocados, tomatoes, kiwi, pineapple, and citrus, which can be higher in histamine or trigger release)
- Good options: apples, pears, watermelon, mango, blueberries, grapes
- Most fresh vegetables (except tomatoes, spinach, eggplant, and avocado)
- Good options: carrots, broccoli, cauliflower, courgette, lettuce, green beans, sweet potatoes
- Gluten-free grains (rice, quinoa, millet, oats)
- Dairy alternatives (coconut milk, rice milk, oat milk—avoid aged cheeses and yoghurt)
- Olive oil and coconut oil
- Herbal teas (not black or green tea)
- Fresh herbs (parsley, coriander, basil)
- Pure, unprocessed honey and maple syrup

Foods to avoid (higher in histamine)
- Aged cheeses
- Processed or smoked meats (ham, salami, bacon, sausages)
- Canned, smoked, or dried fish
- Alcohol (especially wine, beer, champagne)
- Fermented foods (sauerkraut, soy sauce, vinegar, pickles, kombucha)
- Leftovers (histamine builds up in stored foods)
- Vinegar-containing foods (mayonnaise, ketchup, mustard)
Tip:
Always eat foods as fresh as possible, and try to avoid leftovers or anything that’s been sitting out for a while, as histamine levels rise with storage.

How is MCAS diagnosed?
MCAS can be tricky to diagnose—there’s no single test that gives a simple answer. Doctors usually follow a step-by-step approach:
- Check for symptoms in two or more parts of the body (like skin and gut, or lungs and brain) [8].
- Try a “medication trial” with drugs that calm mast cells (like antihistamines). If you feel better, that’s a clue [2].
- Run lab tests to look for high levels of mast cell chemicals in your blood or urine, especially during a flare-up. Tests might include tryptase, methylhistamine, and prostaglandins, but results aren’t always clear-cut [2].
- Rule out other conditions that could explain your symptoms, which might involve extra tests like scans or biopsies[2].

How is mast cell activation syndrome treated?
There’s no cure for MCAS, but symptoms can often be managed. Treatment usually involves:
- Avoiding things that trigger your symptoms (like certain foods, stress, or medications) [9].
- Taking medicines such as antihistamines, mast cell stabilisers, or other drugs prescribed by your doctor [9].
- Carrying an adrenaline injector (like an EpiPen) if you’re at risk of severe allergic reactions [9].
- Some people may need more specialised medicines if usual treatments don’t work[9].

Examples of mast cell stabilisers
An example of a popular mast cell stabiliser that is used in the management of mast cell activation syndrome is ketotifen or Zaditen.
Courier Pharmacy has both the Zaditen 1mg (ketotifen 1mg tablets) and the Zaditen 1mg/5ml oral liquid (ketotifen 1mg/5ml oral liquid).
Both of these different formulations of the popular mast cell stabiliser are available from Courier Pharmacy after completing an online questionnaire.
-
 Zaditen Elixir – Ketotifen 1mg/5ml Elixir, 300mlPrice range: £34.99 through £99.99
Zaditen Elixir – Ketotifen 1mg/5ml Elixir, 300mlPrice range: £34.99 through £99.99 -
 Ketotifen 1mg (Zaditen) tabletsPrice range: £29.99 through £89.99
Ketotifen 1mg (Zaditen) tabletsPrice range: £29.99 through £89.99 -
 Loratadine 10mg TabletsPrice range: £1.99 through £12.99
Loratadine 10mg TabletsPrice range: £1.99 through £12.99
What else should I know about MCAS?
- MCAS can look like other illnesses, so it’s important to work with your doctor for a proper diagnosis.
- Keeping a diary of your symptoms and triggers can help.
- MCAS is different from mastocytosis, which is when there are too many mast cells in the body.
- MCAS can sometimes be linked to other conditions, like irritable bowel syndrome (IBS), Ehlers-Danlos syndrome, or even long COVID [2].

Why does mast cell activation syndrome matter?
Because MCAS can cause so many different symptoms, it often takes time to get the right diagnosis. Raising awareness helps people get the right treatment sooner and improves quality of life.

MCAS in summary
MCAS is a rare condition where certain immune cells, called mast cells, release too many chemicals, leading to a mix of allergy-like symptoms.
It can affect many parts of the body and is tricky to diagnose, but with the proper support and treatment, people with MCAS can manage their symptoms and live well.

What’s the risk of anaphylaxis with MCAS?
People with MCAS are more likely to have severe allergic reactions (anaphylaxis). Warning signs include:
- Swelling of the tongue or lips
- Trouble breathing or swallowing
- Sudden drop in blood pressure, confusion, or fainting
If you’re at risk, you’ll need to carry an adrenaline auto-injector (like an EpiPen) and use it at the first sign of anaphylaxis [1], [2]. Always call for an ambulance after using your injector, even if you feel better

FAQs: What is mast cell activation syndrome? (and other common questions)
Is MCAS the same as an allergy?
No, it’s more complicated. Allergies are usually triggered by specific things (like peanuts or pollen), but all sorts of things can set off MCAS—or sometimes nothing obvious at all.
Can children get MCAS?
Yes, MCAS can affect both children and adults.
Will MCAS go away on its own?
It’s usually a long-term condition, but symptoms can improve with good management.
Why does MCAS make me so tired?
The chemicals mast cells release can affect your whole body, including your brain, leading to fatigue and brain fog.
Is MCAS genetic?
Some mast cell disorders, such as hereditary alpha tryptasemia syndrome (HATS), are genetic and caused by extra copies of a gene called alpha tryptase. MCAS itself might run in families, but scientists are still figuring out exactly how genetics come into play.

The bottom line: What is mast cell activation syndrome?
MCAS is a complex, often misunderstood condition where your mast cells are a bit too sensitive, releasing chemicals that cause a range of symptoms.
It’s not always easy to diagnose or manage, but with the right support and a bit of detective work, you can live well with MCAS.
If you think you might have it, talk to your GP or a specialist or contact us for a FREE consultation.
This information is for general guidance only. For medical advice, please consult your doctor or healthcare provider.

References
- Mast Cell Action (n.d.) About MCAS. Available at: https://www.mastcellaction.org/about-mcas (Accessed: 1 August 2025).
- Özdemir Ö, Kas?mo?lu G, Bak A, Sütlüo?lu H, Sava?an S. Mast cell activation syndrome: An up-to-date review of literature. World J Clin Pediatr. 2024 Jun 9;13(2):92813.
- Picard, M. et al. (2018) ‘Mast Cell Activation Syndromes: Pathophysiology, Diagnosis, and Treatment’, Immunology and Allergy Clinics of North America, 38(3), pp. 505–525.
- Özdemir, Ö., 2005. Immunosurveillance function of human mast cell?. World Journal of Gastroenterology, 11(44), p.7054.
- Afrin LB. Presentation, diagnosis, and management of mast cell activation syndrome. 2013; 155-232 Available from: https://experts.umn.edu/en/publications/presentation-diagnosis-and-management-of-mast-cell-activation-syn
- Sánchez-Pérez, S., Comas-Basté, O., Veciana-Nogués, M.T., Latorre-Moratalla, M.L. and Vidal-Carou, M.C., 2021. Low-histamine diets: is the exclusion of foods justified by their histamine content?. Nutrients, 13(5), p.1395.
- Vlieg-Boerstra, B.J., Van der Heide, S., Oude Elberink, J.N., Kluin-Nelemans, J.C. and Dubois, A.E., 2005. Mastocytosis and adverse reactions to biogenic amines and histamine-releasing foods: what is the evidence. Neth J Med, 63(7), pp.244-9.
- Molderings, G.J., Homann, J., Brettner, S., Raithel, M. and Frieling, T., 2014. Mast cell activation disease: a concise practical guide for diagnostic workup and therapeutic options. Deutsche medizinische Wochenschrift (1946), 139(30), pp.1523-34.
- Valent, P., Akin, C., Nedoszytko, B., Bonadonna, P., Hartmann, K., Niedoszytko, M., Brockow, K., Siebenhaar, F., Triggiani, M., Arock, M. and Romantowski, J., 2020. Diagnosis, classification and management of mast cell activation syndromes (MCAS) in the era of personalized medicine. International journal of molecular sciences, 21(23), p.9030.
- Medical Mojo. MCAS: Symptoms, Diagnosis and Management.